
This article is more than
9 year oldHis patient sits still but her face contorts with pain in a hospital ward in Namibia's capital, Windhoek.
The wards are busy on this Monday morning and scores are waiting to be treated in the emergency department.
The 25-year-old is slight but has a quiet confidence about him and people here in Katutura hospital seem to trust him.
He was one of 37 in the first class of locally trained doctors to graduate earlier this year.

Until 2010, when the country's first medical school opened, would-be doctors had to travel abroad - to South Africa, Russia, Cuba, Algeria and China - to be educated.
So Dr Murangi is in the vanguard of something which could see a transformation in the health service here.
Namibia is a vast country but has a population of just 2.5 million, which is scattered in mostly rural and arid regions. This means that doctors are concentrated in urban areas and sometimes people have to travel a long way to get treated.
This morning some have travelled more than 50km (30 miles) to get to Katutura hospital. They wait quietly, but the doctors are feeling the pressure.

"Sometimes the workload can get quite overwhelming, you find that you have many patients to see and you get fatigued. You don't have time to rest. This can really negatively affect patient care," Dr Murangi tells the BBC.
But things are improving and many here believe that the country's new medical school presents a lasting solution to the problem of a lack of doctors.

Source: WHO Global Health Observatory

The World Health Organization (WHO) has said that the shortage of medical staff in the public health sector here has hindered Namibia's development.
One of the reasons behind the shortage is that it was only since independence from South Africa's apartheid government in 1990 that health services were made available to the majority of people in Namibia, experts say.
A high HIV rate, shortage of medication in rural hospitals, limited training facilities, old infrastructure and a lack of equipment to treat patients have compounded the problem.
But Deputy Health Minister Juliet Kavetuna, who describes the sector as "fragile", says she believes the country is now on the right track.

"We are now training more doctors than ever," she says.
"Our research has shown that in our hospitals we need multiple disciplines including pharmacists, physiotherapists and dentists to work alongside doctors.
"We believe we are now taking steps in the right direction."
For years Namibia's government had to spend a lot of money funding students to train abroad.
Some of the graduates then moved into private healthcare, which can pay more and offer better working conditions, but are beyond the reach of most of the population.
But with the new graduates this is expected to change.
"These graduates are the pride of Namibia.
"Many of our doctors that we get from abroad want to stay in Windhoek but our home-grown doctors, because they know our healthcare system, want to go and work outside in rural areas - that will be good for our people," says the deputy health minister.
Dr Murangi, the eldest of four children, graduated with the help of government funding, and said he would not have become a doctor otherwise.
For many families, a medical degree is simply unaffordable and Dr Murangi says he was fortunate to receive a full scholarship.
"My family were very proud when I graduated, they've even encouraged me to study further if possible. It means a lot to all of us."
And what of those following in his footsteps?
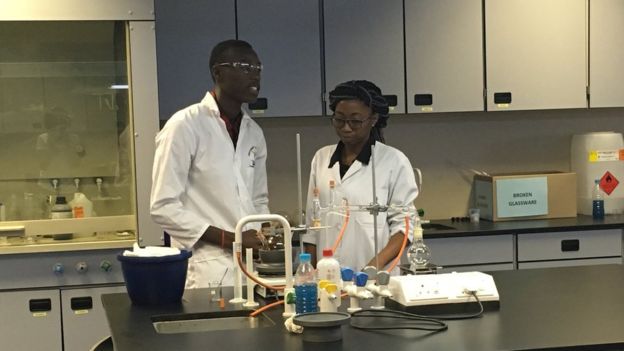
A short distance from the bustling hospital, Namibia's future doctors are huddled together in a well kitted-out laboratory learning about neurological disorders and how to diagnose them.
The University of Namibia's medical sciences centre started with 50 students but now 400, mostly Namibians, are enrolled here, and building work continues alongside the teaching.
The school complex is grand with high, sleekly finished red and grey walls. The modern architecture stands out among the somewhat run-down houses in the area.
Inside I sit at the cafeteria with some first year students, aged between 18 and 19, who were on a break between between classes.
"It's better to study in a place with which you are familiar. I do want to travel abroad to learn more but this is where my skills are most needed," says Nzinga Mwanachilenga.

Another, Ndapandula Hamunime, tells me she studied in Hungary for a year and is now back home.
"I think the programme here is more suited to the social setting of Namibia and I think in the end that will help patients.
"From very early in the programme, we work very closely with communities and we build relationships with them," she says.
But a medical degree does not come cheap. At Cape Town's prestigious university, where Namibia's government regularly sends its students, tuition is about 64,500 rand ($4,640; £3,800). The degree at UNAM's costs about the same.
"I think there are many people that are interested in studying medicine but they couldn't because that course wasn't offered here and they couldn't afford the extra costs of studying overseas, so having our own university helps," says Jennifer Muyenga-Muyenga.
"It also means I can be with my family."
These "home-grown" doctors, as they have been nicknamed, hope they can offer more to patients but add they will need the continued support of internationally trained doctors.
Namibia's health problems are far from over but many are hopeful that quality health will no longer be seen as a luxury, beyond the reach of many.